A total hip replacement (or total hip arthroplasty) is a successful operation for end-stage hip arthritis. The most common indication for a hip replacement is osteoarthritis, which is a degenerative disease that causes progressive loss of joint cartilage. Patients with hip arthritis often feel groin or buttock pain with walking and rising from a seated position. In addition, patients describe hip stiffness and difficulty with normal day-to-day activities such as putting on socks or shoes.
Other indications for a hip replacement include rheumatoid arthritis, post-traumatic arthritis, avascular necrosis of the hip, and certain hip fractures.
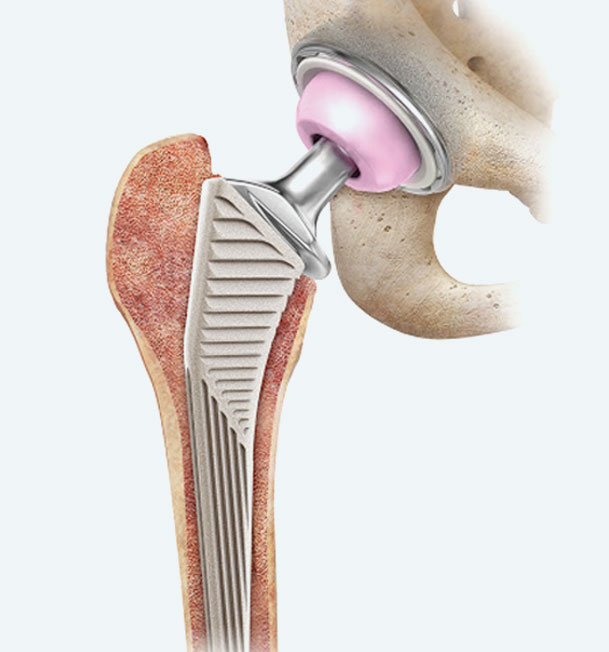
The goal of a total hip replacement it to replace the damaged joint with an artificial joint (prosthesis) to improve the pain and disability associated with arthritis.
After a hip replacement, most patients experience significant pain relief and improvements in walking, sleeping, flexibility, and other daily activities.