Revision (re-do) total hip and knee replacements involve removing the original artificial joint (prosthesis) and implanting new components. Surgery is generally more complicated and associated with an increased risk of postoperative complications. In addition, recovery is less predictable and typically prolonged compared to primary (first time) surgery.
Frequently Asked Questions
What is the most common reason for a Revision Total Hip Replacement?
What gets replaced in a Revision Total Hip Replacement?
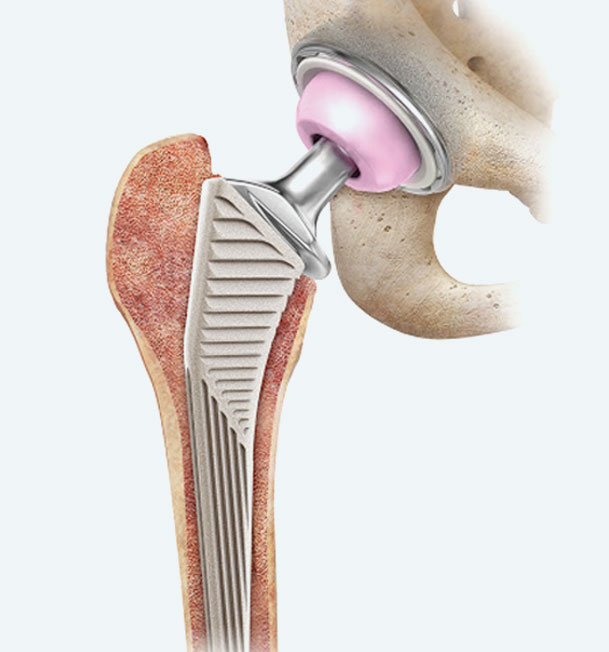
In some situations, revision surgery may only require exchange of the modular (replaceable) components including the femoral head (ball) and acetabular liner (plastic socket). However, in more complicated scenarios it may be required to completely remove (and replace) the metal acetabular component (socket), femoral component (stem), or both.
In the setting of an infection, two separate operations (two-stage revision) may be required to eradicate the infection. The first stage involves implantation of a temporary “spacer” followed by a course of antibiotics. After a successful course of antibiotics, the final components can then be safely implanted in the second stage.
What is the most common reason for a Revision Total Knee Replacement?
What gets replaced in a Revision Total Knee Replacement?
Revision total knee replacement typically involves replacement of the femoral component (end of thigh bone), tibial component (top of shin bone), and plastic liner. On some occasions it may be possible to just exchange the modular (replaceable) plastic liner.
In the setting of an infection, two separate operations (two-stage revision) may be required to eradicate the infection. The first stage involves implantation of a temporary “spacer” followed by a course of antibiotics. After a successful course of antibiotics, the final components can then be safely implanted in the second stage.
When should I get a revision hip or knee replacement?
The decision to proceed with a revision hip or knee replacement can be complex. It is important to have a formal discussion with your surgeon to determine if you require a revision operation.
It is important to obtain your medical records (including your previous operative report) if your appointment is with a different surgeon to the one who performed your original hip or knee replacement.
What is the expected recovery?
The majority patients who undergo a revision hip or knee replacement are admitted to the hospital overnight. Some patients may be candidates to be discharged the same day of surgery. Recovery after a revision hip or knee replacement is typically longer and less predictable. After surgery you will be assessed by a physiotherapist to ensure that you can mobilize and climb the stairs safely. You will be given a prescription for pain medication and blood thinners prior to discharge.
Your first post-operative appointment will be approximately 2-weeks after surgery in the fracture clinic to check your wound and review your progress.
The second follow-up appointment will be approximately 6 weeks after surgery. A clinical review and x-ray will be performed at that time.
It is typical to require a walker or crutches for the first 2-6 weeks after surgery. It is often advisable to transition to a cane after you have stopped using a walker. Most patients are comfortable with normal day-to-day activities 6-8 weeks after surgery. However, this is variable and depends on the complexity of the revision operation. Initial recovery can be longer in some cases.
The average recovery following revision hip or knee replacement is less predictable but is approximately 6 months. However, it can take up to 12-18 months after surgery to regain full strength.
When can I go back to work?
When can I drive?
When can I fly or travel after my revision hip or knee replacement?
Travel should be delayed for 6 weeks after surgery. Long distance travel and flying increases the risk of developing a blood clot early in the post-operative period.
If flying is essential prior to 6 weeks, it is recommended that you get up and move every hour on the plane. You will also require a prescription blood thinner.
Do I need antibiotics before a dental procedure?
You do not require any antibiotics before a routine dental procedure.
The Canadian Orthopaedic Association (COA), Canadian Dental Association (CDA), and the Association of Medical Microbiology and Infectious Disease (AMMI) have reviewed the best available research and have provided clear guidance on this.
Infection
The risk of a (deep) prosthetic joint infection is approximately 1% following primary (first-time) knee replacements and up to 5-10% of revision (re-do) knee replacements. You will receive a dose of IV antibiotics before and after surgery to decrease the risk of infection. Prolonged antibiotics after surgery have not been shown to provide additional benefit and are usually not required.
Symptoms of a prosthetic joint infection include swelling, redness, wound drainage and increasing pain. Patients can also experience systemic symptoms such as a fever. Please contact your surgeon and/or go to the emergency department if you believe you are developing an infection.
Deep prosthetic joint infections may require IV antibiotics and multiple operations in order to eradicate the infection. Some or all of the components may need to be removed or exchanged.
Superficial skin infections are more common and can be usually treated with a course of oral antibiotics.
Dislocation (Revision Total Hip Replacement)
A dislocation occurs when the femoral head (ball) comes out of the acetabulum (socket). The risk of dislocation is approximately 1-2% following a primary (first-time) total hip replacement and up to 10% following a revision (re-do) hip replacement.
Most dislocations occur in the first 6-12 weeks after surgery. Recurrent dislocations may require revision surgery to stabilise the hip joint.
Periprosthetic Fracture (Revision Total Hip Replacement)
Management depends on the location and severity of the fracture. Some periprosthetic fractures can be treated non-operatively. Other periprosthetic fractures require surgery to fix the fracture +/- revision (re-do) hip replacement.
Leg length discrepancy (Revision Total Hip Replacement)
One of the goals of revision hip replacement surgery is to restore equal leg lengths after surgery. However, it is occasionally necessary to make your leg slightly longer to optimise stability of your hip and prevent dislocation.
Knee stiffness (Revision Total Knee Replacement)
Knee stiffness can be a problem after a revision total knee replacement. It is normal for your knee to be stiff and painful immediately after surgery. However, it is very important to work on your knee range of motion after surgery to prevent permanent stiffness. Expected range of motion is approximately from 0 (completely straight) to 120 degrees.
If you develop permanent stiffness, you may require surgery to manipulate the knee and break up the scar tissue (manipulation under anaesthesia). In some cases, a second revision (re-do) operation may be necessary to improve flexibility.
Extensor mechanism injury (Revision Total Knee Replacement)
Your extensor mechanism attaches your quadriceps muscle to the proximal tibia and allows you to straighten you knee when bent. It is made up of the patella tendon, patella, and quadriceps tendon and is essential for adequate function of your knee.
An extensor mechanism injury is a potential complication of a revision knee replacement. Treatment depends on severity but may involve immobilization in a knee brace or reconstructive surgery.
Revision Surgery
There is an increased risk of a (repeat) revision total hip or knee replacement after a revision procedure. Common indications for revision surgery are listed above.
Blood clot
A deep vein thrombosis (DVT) is a blood clot that can develop in the leg veins after surgery. DVTs that occur above the knee can be dangerous as they can dislodge and form a blood clot in the lungs called a pulmonary embolism (PE). This is a rare but serious condition which can be life threatening.
All patients receive medication to reduce the risk of a blood clot after surgery. The type of medication varies depending on the individual risk factors of each patient. If you have had a blood clot in the past it is important to inform your surgeon prior to surgery.
Damage to major nerve or blood vessels
Damage to major nerves, such as the sciatic nerve (after revision total hip replacement) and common peroneal nerve (after revision total knee replacement) can occur during surgery. Although it is a rare complication, the risk is increased with revision surgery compared to primary surgery. This can lead to a partial paralysis such as a “foot drop” where there is inability to lift the front part of the foot. Recovery can be prolonged and incomplete.
Major blood vessel damage is also extremely rare but can necessitate emergency blood transfusion and vascular repair in some cases.